Lactiplantibacillus plantarum DSM 9843
Lactobacillus as a genus
Lactic acid bacteria is a functional group of bacteria. The term is used by Food microbiologists as a collective term for bacteria able to ferment carbohydrates in foods to lactic acid. They typically occur spontaneously in fermented foods and consist of several different bacterial families and genus such as the family Lactobacillaceae and the genus Lactobacillus.
Lactobacillus is a genus of bacteria consisting of more than 90 defined species, all able to ferment
carbohydrates into carboxylic acids, mainly lactic acid. The Lactobacillus species have been divided into three functional groups based on fermentation function; Group I (obligate homofermentative) which ferments hexoses to lactic acid but cannot ferment gluconate or pentoses, Group II (facultative heterofermentative) which in addition to hexose also ferments pentoses and/or gluconate and finally Group III (obligate heterofermentative) which ferments hexoses to lactic acid, acetic acid and or ethanol and carbon dioxide.
Lactobacillus plantarum
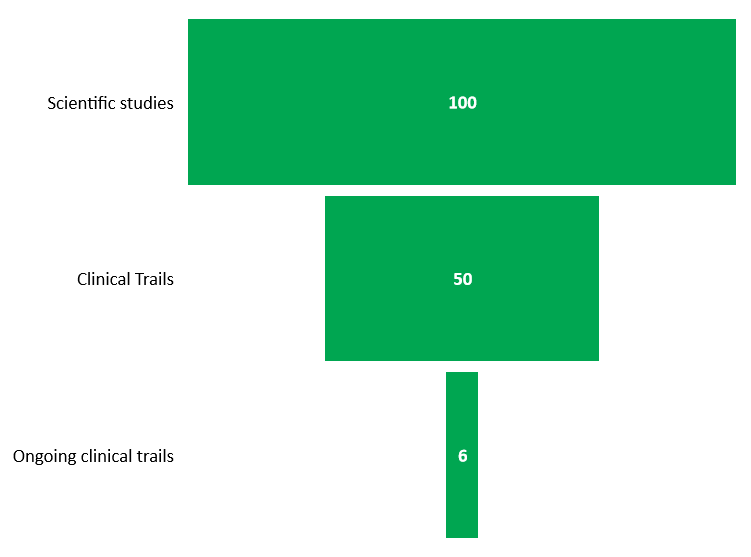
Lactobacillus plantarum DSM 9843 – >100 studies and >50 clinical studies, 6 ongoing studies.
Lactobacillus plantarum has one of the largest genomes, the type organism WCSF1 contains 3052 genes (1), known among lactic acid bacteria which makes it highly versatile for instance helping it to grow between pH 3.4-8.8 (2) and in temperatures from 12 to 40 degrees C (3). L. plantarum belongs to group II of Lactobacillus and is facultative heterofermentative which in addition to hexose also ferments pentoses and/or gluconate to Lactic acid (1). The organism is used commercially as silage inoculant where they quickly become dominant in culture and produce both lactic and acetic acid. It is commonly found in food products such as milk products and fermented foods such as kimchi, sauerkraut, and sourdough.
- L. plantarum DSM 9843 was isolated from human intestinal mucosa (4).
- The strain is robust. It possesses wide pH tolerance and grows at pH between 4 and 8, it can survive down to pH2 and up to 9.0 (5).
- The strain can be considered halo-tolerant and can be grown in 6% NaCl and survive in 16% NaCl, it also grows in the presence of bile salts up to 2% (5).
- L. plantarum attaches to human mucose cells in vitro depending on a mannose-binding adherence (6).
- In addition to being important for colonization this ability is also important for its immune modulating ability (7) and ability to decrease bacterial translocation through the intestinal wall (8).
Example of studied health effects
IBS (9), (10), (11) . Nobaek et al found that administering a fruit drink containing L. plantarum DSM 9843 significantly reduced subjectively experienced bloating. Niedzelin et al, utilizing the same delivery format, found that IBS symptoms decreased. Finally, Ducrotte et al. found L. plantarum DSM 9843 to significantly decrease both pain severity and incidence as well as bloating.
Several mechanisms of action sources have been discussed for IBS
- Luminal interactions (11). Since it has been observed that abdominal pain intensity is reduced more in vegetarians it suggests the symptomatic effect can be related to interactions between the luminal content or that the strain affects the luminal metabolism of nutrients.
Nitric Oxide generates intestine motility (10). L. plantarum can catabolize arginine thus generating nitric oxide. It has been suggested that nitric oxide may exert a positive effect on the motility of the large and small intestines.
Suppression of excessive inappropriate inflammation (12). L. plantarum increased IL-10 synthesis and secretion in macrophages and T-cells derived from the colon. IL-10 is a beneficial cytokine for inappropriate inflammation as it has immunosuppressive effects on Th1 cells. L. plantarum in the commensal gut flora could therefore reduce inflammatory responses in the colon. An environment with L. plantarum in the gut flora will be richer in IL-10 which contributes to amelioration of excessive inappropriate inflammation.
Antimicrobial property (14), (17)
- Diarrhea, antibiotic and Clostridium difficile associated (13), (14). Lönnermark et al found that hospitalized patients on antibiotics drinking fruit drink containing L. plantarum DSM 9843 had significantly fewer loose or watery stools than a control group which received a placebo fruit drink. Wullt et al saw a trend that recurrence of infection episodes was lowered for patients receiving L. plantarum DSM 9843 as compared with a placebo group.
Coronary artery disease (15). Bukowska et al found, In a human trial on men with slightly elevated cholesterol levels, that concentration of total cholesterol and LDL-cholesterol were deceased in the active L. plantarum DSM 9843 group as compared with placebo.
Development of Immune system (16) and inflammation (12). Rask et al found that L. plantarum DSM 9843 seemed to activate acquired T-cell immunity by increasing expression on activation markers and memory cell markers. In the cholesterol level study by Bukowska it was also found that fibrinogen levels were significantly reduced in the active L. plantarum DSM 9843 group showing a lowered systemic inflammation status of the individuals.
1. Kleerebezem, Michiel; et al. (2003). ”Complete genome sequence of Lactobacillus plantarum WCFS1”. Proceedings of the National Academy of Sciences. 100 (4): 1990–5. Bibcode:2003
2. E Giraud, B Lelong and M Raimbault. 1991. Influence of pH and initial lactate concentration on the growth of Lactobacillus plantarum Applied Microbiology and Biotechnology. 36(1):96–99
3. Martino, Maria Elena; Bayjanov, Jumamurat R.; Caffrey, Brian E.; Wels, Michiel; Joncour, Pauline; Hughes, Sandrine; Gillet, Benjamin; Kleerebezem, Michiel; van Hijum, Sacha A. F. T.; Leulier, François (2016). ”Nomadic lifestyle of Lactobacillus plantarum revealed by comparative genomics of 54 strains isolated from different habitats”. Environmental Microbiology
4. Molin, G., Jeppsson, B., Ahrné, S., Johansson, M.-L., Nobaek, S., Ståhl, M., and Bengmark, S. (1993). Numerical taxonomy of Lactobacillus spp. associated with healthy and diseased mucosa of the human intestines, J. Appl. Bacteriol. 74: 314-323.
5. Melgar-Lalanne, G., Rivera-Espinoza, Y., Farrera-Rebollo, R. and Hernández-Sánchez, H. (2014). Survival under stress of halotolerant lactobacilli with probiotic properties. Revista Mexicana de Ingeniería Química 13: 323-335.
6. Adlerberth, I., Ahrné, S., Johansson, M-L., Molin, G., Hanson, L-Å., and Wold, A.E. (1996). A mannose-specific adherence mechanism in Lactobacillus plantarum conferring binding to the human colonic cell line HT-29, Appl. Environ. Microbiol., 62: 2244-2251.
7. McCracken, V.J, Chun, T., Baldeón, M.E., Ahrné, S., Molin, G., Mackie, R.I. & Gaskins, H.R. (2002). TNF-a sensitizes HT-29 colonic epithelial cells to intestinal lactobacilli. Experimental Biology and Medicine 227: 665-670.
8. Mangell, P., Lennernäs, P., Wang, M., Olsson, C., Ahrné, S., Molin, G., Thorlacius, H. and Jeppsson, B. (2006). Adhesive capability of L plantarum 299v is important for preventing bacterial translocation in endotoxaemic rats. APMIS 114: 611-618.
9. Nobaek, S., Johansson, M-L., Molin, G., Ahrné, S., and Jeppsson, B. (2000). Alteration of intestinal microflora is associated with reduction in abdominal bloating and pain in patients with irritable bowel syndrome, Am. J. Gastroenterol. 95: 1231-1238.
10. Niedzielin, K., Kordecki, H., and Birkenfeld, B. (2001). A controlled, double-blind, randomized study on the efficacy of Lactobacillus plantarum 299v in patients with irritable bowel syndrome, Eur. J. Gastroenterol. Hepatology 13: 1143-1147.
11. Ducrotté, P., Sawant, P. and Jayanthi, V. (2012). Clinical trial: Lactobacillus plantarum 299v (DSM 9843) improves symptoms of irritable bowel syndrome. World Journal of Gastroenterology 18: 4012-4018.
12. Pathmakanthan S, et al. Beneficial in vitro immunomodulation in cells extracted from inflamed human colon. Journal of Gastroenterology and Hepatology (2004) 19, 166-173
13. Lönnermark, E., Friman, V., Lappas, G., Sandberg, T., Berggren, A. and Ingegerd Adlerberth (2010). Intake of Lactobacillus plantarum reduces certain gastrointestinal symptoms during treatment with antibiotics. Journal of Clinical Gastroenterology
14. Wullt, M., Johansson Hagslätt, M.-L. and Odenholt, I. (2003). Lactobacillus plantarum 299v for the treatment of recurrent Clostridium difficile-associated diarrhoea: A double-blind placebo-controlled trial. Scandinavian Journal of Infect. Dis. 35: 365-367.
15. Bukowska, H., Pieczul-Mróz, J., Jastrzebsk, K., Chelstowski, K., and Naruszewicz, M. (1998). Significant decrease in fibrinogen and LDL-cholesterol levels upon supplementation of the diet with Lactobacillus plantarum (ProViva) in subjects with moderately elevated cholesterol concentrations, Atherosclerosis, 137: 437-438.
16. Rask, C., Adlerberth, I., Berggren, A. and Lazou Ahrén, I. and Wold, A.E. (2013). Differential effect on cell-mediated immunity in human volunteers after intake of different lactobacilli. Clinical and Experimental Immunology 172: 321–332.
17. Klarin, B., Wult, M., Palmquist, I, Molin, G., Larsson, A. & Jeppsson, B. (2008). Lactobacillus plantarum 299v reduces colonisation of Clostridium difficile in critically ill patients treated with antibiotics. Acta Anaesthesiologica Scandinavica 52: 1096-1102.